A Decade Away or Sooner Than We Think?
For decades, the global medical community has faced a persistent and deeply human problem: a chronic shortage of transplantable organs. Each year, thousands die while waiting on transplant lists. Traditional methods of organ donation cannot keep up with demand. In this context, 3D bioprinting has emerged as one of the most tantalizing promises of modern medicine, a technology that could one day print human organs on demand, customized to the patient and free from the risk of rejection. While the concept once sounded like science fiction, today it sits on the edge of clinical plausibility. But is the dream truly within reach?
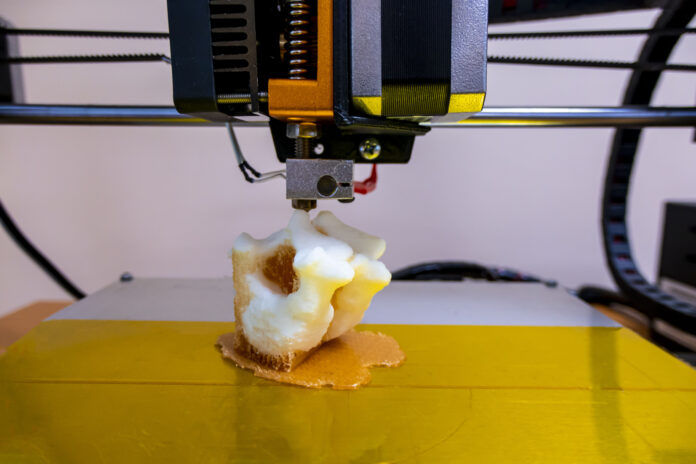
3D bioprinting is a process in which living cells, biomaterials and growth factors are precisely deposited, layer by layer, to build three-dimensional tissue structures. Using a digital blueprint, these printers can create complex biological architectures such as skin, cartilage, blood vessels and, eventually, entire organs like kidneys or hearts. Unlike conventional 3D printing, which uses plastics or metals, bioprinting employs “bioinks” composed of cells and hydrogel-based scaffolds, mimicking the structure and function of real
human tissue.
From Labs to Living Systems
In controlled laboratory settings, scientists have already printed miniature livers, cardiac patches, retinal tissues and rudimentary lung structures. These constructs are used for drug testing, toxicology studies and disease modeling, reducing reliance on animal testing and providing more accurate human-relevant results. The commercial pharmaceutical industry has embraced bioprinted tissue as a powerful research tool, with some printed liver models
now able to survive and function for over a month in a petri dish.
But printing functional, full-scale human organs is a far greater challenge. It’s not just about shape—it’s about function. An organ must replicate highly specialized cellular interactions, vascular networks for blood flow, and mechanical dynamics like pulsation or filtration. For instance, a bioprinted heart must beat continuously with synchronized electrical signals and withstand the pressure of circulating blood. A kidney must filter waste, manage fluid balance
and respond to hormonal signals.
The biggest technical hurdle remains vascularization, the process of integrating tiny blood vessels throughout the organ to keep cells alive. Without proper blood supply, thick tissues die before they can mature. Researchers are now developing new bioinks, advanced printing strategies and self-assembling tissue techniques to solve this problem. Some are turning to machine learning to simulate and optimize the complex design parameters required for successful organ function.
Another challenge is time. Even with a perfect blueprint, it can take hours or days to print a single organ. Post-print maturation in bioreactors can take weeks. And because each patient’s cells may be used, personalization adds another layer of logistical complexity. Yet as printing speeds improve and stem cell engineering becomes more advanced, these timelines are steadily shrinking.
Regulatory and ethical dimensions are also critical. How do we ensure safety, standardization and traceability of bioprinted organs? Who will have access to them, and at what cost? Will the ability to print organs open doors to unethical uses, like enhancement or black-market demand? Policymakers and bioethicists are already grappling with these questions, though
the technology has not yet reached mainstream clinical deployment.
Nonetheless, progress continues. In 2022, researchers at Tel Aviv University successfully printed a tiny, beating heart with blood vessels, made entirely from a patient’s cells. In the United States, companies like Organovo and United Therapeutics are working with regulatory bodies to advance bioprinted tissue for therapeutic use. In South Korea, printed cartilage implants are already being tested in clinical trials. Closer to home, several Asian
research centers are making headway in printing corneal tissue and pancreatic islets, pushing the boundaries of regenerative medicine.
Looking ahead, 3D bioprinting may not fully replace organ donation anytime soon, but it is likely to become a crucial part of a hybrid approach. Surgeons may one day use printed patches to repair damaged hearts or livers. Bioprinted scaffolds could help regenerate bone or nerve tissues. In the next ten years, it is plausible that composite organs, partially printed and partially scaffolded with natural tissue, may enter early clinical practice.
For healthcare systems in emerging economies, the implications are profound. If scalable, bioprinting could reduce dependence on foreign organ donation networks, limit transplant tourism, and provide more affordable, locally produced solutions for chronic disease treatment. Educational institutions must begin training a new generation of professionals who can navigate the intersection of biology, engineering and digital technology. Public awareness
campaigns can help manage expectations and prepare communities for the ethical dilemmas ahead.
The idea of printing life may still sound distant, but the building blocks are already in place. What was once theoretical is becoming technical. What was once unimaginable is becoming inevitable. The pace of innovation is fast enough to suggest that 3D bioprinting may no longer be a miracle ten years away it may be a revolution arriving right on time.